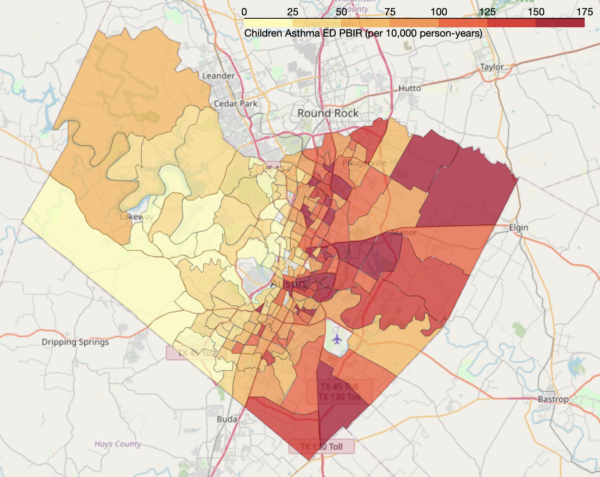
AUSTIN, Texas – Kids living in Travis County are hospitalized for asthma at a significantly higher rate than U.S. children overall, with the highest rates of emergency room visits and hospitalizations across the county occurring in eastern Travis County, according to the first study of its kind published in The Journal of Allergy and Clinical Immunology.
The Centers for Disease Control and Prevention (CDC) estimated 5.1 million U.S. children had asthma in 2019. A chronic condition affecting the airways in lungs, asthma disproportionately affects people of color and those living in poverty.
To better understand how asthma emergency room and hospitalization incidence varies within Travis County, population health researchers at Dell Medical School at The University of Texas at Austin used publicly available health data to compare the rates of asthma-related emergency room visits and hospitalizations among all Travis County residents in 2016 and 2017.
The study showed that about 16 out of every 10,000 kids younger than 18 in Travis County are hospitalized for asthma per year, compared with about 10 out of 10,000 children elsewhere – a rate 60% higher than the national average.
The vast majority of neighborhoods with the highest rates of asthma-related emergency room visits were east of Interstate 35.
The study, the first of its kind to compare asthma data between neighborhoods instead of ZIP codes, also yielded an unexpected result about asthma among Latino populations.
“When the team examined asthma ER visit rates by neighborhood, we were surprised to find such a heavy burden of asthma in areas where most ethnic minority residents are Latinx, primarily of Mexican origin – a population traditionally thought to be at very low risk of asthma,” according to study author Elizabeth Matsui, M.D., MHS, professor of population health and pediatrics. A 2018 study showed that 5.3% of Mexican Americans living in the U.S. have asthma, compared with 7.6% of non-Latino/Hispanic whites.
The reasons for such high rates of asthma-related illness in Travis County, and specifically for the high rate of Latinx residents affected by asthma, are not yet fully understood, said Matsui.
Previous research shows that areas with higher poverty rates and a greater concentration of populations of color have higher rates of asthma emergency room visits, but that only explains part of the results, according to the study.
Matsui’s team concluded that in addition to identifying the factors associated with populations of color that increase the risk of asthma emergency room visits, researchers must delve deeper into other factors driving these differences.
“Even though racial and ethnic disparities in asthma have been recognized for decades, scientists have not yet made a dent in these disparities, in part because researchers tend to chase after biological explanations instead of focusing on contextual factors that go along with being a member of a minority group – factors stemming from structural racism, which include things like the physical and social environment,” Matsui said.
To connect environmental inequities to racial and ethnic disparities in health conditions such as asthma, the Center for Health and Environment: Education and Research (CHEER) was established earlier this year as a hub for multidisciplinary environment health sciences research and learning. Led by Matsui, CHEER combines experts from Dell Med, the Steve Hicks School of Social Work, College of Pharmacy, Cockrell School of Engineering and College of Natural Sciences at UT Austin.
In an effort to better understand the role of neighborhood and home environmental exposures affecting asthma disparities, CHEER recently launched the Texas Home Assessment of Asthma and Lung Exposures (TexHALE), a new study informed by input from a community advisory board.
“Our hope is that CHEER will help to identify the best ways we can intervene to shrink these health disparities,” said Matsui.
Study co-authors are R.A. Zarate, M.A., M.Ed., doctoral candidate at UT Austin’s College of Education; Corwin Zigler, Ph.D., associate professor of women’s health at Dell Med and associate professor of statistics and data sciences at UT’s College of Natural Sciences; and Catherine Cubbin, Ph.D., professor and associate dean for research at the Steve Hicks School of Social Work.